Is Hashimoto's Disease Genetic? Unraveling the Potential Link Between Hashimoto's and Family History
"The content below is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition."
Sudden and unexplained weight gain, depression, fatigue, and body aches are just some of the most common symptoms of Hashimoto’s disease.
If you have a close family member who’s been diagnosed with Hashimoto’s, you may be wondering, is Hashimoto’s genetic?
While many look to genetics as an indicator of future health concerns, the answer is not always as straightforward as one would like.
Hashimoto’s disease can have a combination of contributing factors, including your family tree.
This guide unravels the genetic and environmental factors that can help determine your potential risk of developing Hashimoto’s disease.
Table of Contents
Is Hashimoto’s Genetic?
Before we jump into answering if Hashimoto’s disease is genetic, we first need to understand what it is and how it can affect your body.
Hashimoto's disease, named after Dr. Hakaru Hashimoto, who identified it in 1912, is also commonly known as:
- Hashimoto's thyroiditis
- Chronic lymphocytic thyroiditis; or
- Chronic autoimmune thyroiditis
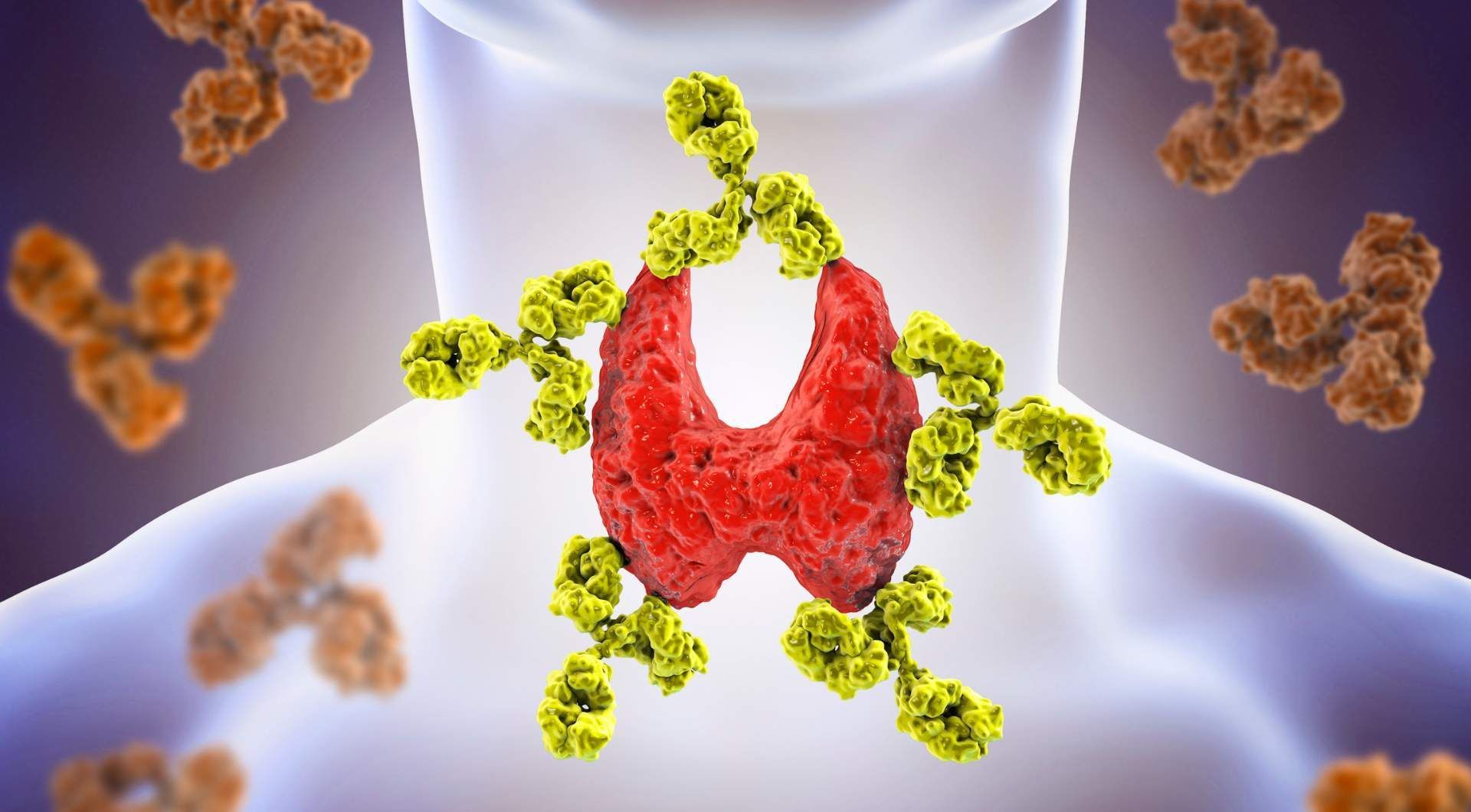
Hashimoto’s is a chronic autoimmune disorder that affects the thyroid gland, a small butterfly-shaped gland that’s smaller in the middle and bows out around either side of the base of the neck around the windpipe or trachea.
The thyroid produces hormones that control the speed of your metabolism and help your body convert the food you consume into energy. Most people think your metabolism only controls weight gain or loss, but this process affects every organ in your body, including your heart and brain.
It’s your immune system's job to protect your body from bacteria, parasites, viruses, and cancerous cells. An autoimmune condition is caused when the immune system attacks healthy tissues in your body instead of protecting it.
In Hashimoto's disease, immune-system cells attack the healthy tissue of the thyroid, keeping it from producing enough thyroid hormone for your body and slowing down your metabolism, also called hypothyroidism.
Though doctors are still unclear if Hashimoto's disease is hereditary because of the many genetic and environmental factors that may be involved, studies have found principal autoimmune disease genes that can cluster in families.
So having a close relative with Hashimoto's disease or another autoimmune disorder can likely increase a person's risk of developing the condition.
Fueling with the right nutrients can help keep your immune system and thyroid working harmoniously.
At
HealthierU, Dr. Donna Sergi can create a holistic nutrition treatment plan designed to help manage Hashimoto's symptoms. Schedule a free consultation today to discover the power of holistic nutrition.
6 Genes Associated With Susceptibility for Hashimoto’s Disease
While the exact cause of Hashimoto’s remains unknown, studies have reported solid evidence that a major genetic influence exists that can predispose one to develop hypothyroidism.
These six genes, called thyroid autoantibodies (TAbs) were found in common and when present in conjunction with other environmental factors, may contribute to the development of Hashimoto’s disease.
#1: Human Leukocyte Antigen (HLA) Genes
Human Leukocyte Antigen (HLA) genes play a major role in the susceptibility to Hashimoto’s disease.
HLA genes contain molecules called glycoproteins that determine the immune system response.
Though data on HLA genes in Hashimoto’s cases have been less definitive, studies have found a genetic association of Hashimoto’s, with three specific HLA genes in Caucasians.
Even a
study among mice found those with a certain HLA gene were susceptible to developing severe cases of Hashimoto’s disease while mice without the gene were resistant to the condition.
#2: Protein Tyrosine Phosphatase Non- Receptor-Type 22 (PTPN22) Gene
The most recently identified immune-regulatory gene associated with Hashimoto’s disease is a genetic variation of the protein tyrosine phosphatase non-receptor-Type 22 gene (PTPN22).
PTPN22 is composed of mostly lymphocytes, also known as T-cells, the germ-fighting white blood cell in the immune system.
When a genetic variation is present in PTPN22, it can decrease the frequency and efficacy of activating T-cells against fighting disease.
One study of Hashimoto’s patients reported a significant association between a specific genetic variation in PTPN22 and the autoimmune disease.
In another small group
study of patients with Hashimoto’s disease and autoimmune diabetes, the impaired T-cell activation caused by PTPN22 was determined in 50% of patients compared with only 14% in healthy controls.
#3: Thyroglobulin Gene
The thyroglobulin gene serves as the storage gene for thyroid hormones in healthy people and those with Hashimoto’s disease or other thyroid disorders.
A
study of Hashimoto’s patients revealed if the thyroglobulin gene possesses one of four out of a possible 14 specific genetic variations, it can cause the thyroglobulin gene to release only small amounts of the hormone into the bloodstream making it an easy target for an autoimmune response.
#4: Cytotoxic T Lymphocyte Antigen-4 (CTLA-4) Gene
The CTLA-4 gene is the second major immune-regulatory gene related to Hashimoto’s disease.
The CTLA-4 gene activates T-cell receptors to interact with T-cells, but certain genetic variations of CTLA-4 can reduce its function and cause it to ultimately suppress T-cell activation.
Remember, if your body is a castle, your T-cells are the army that protects it.
So a reduced inhibition of T-cells means some of your soldiers suddenly can’t be mobilized to defend you, increasing your susceptibility to developing Hashimoto’s disease.
Though other
genetic variations of the CTLA-4 genes have been identified as significantly associated with Hashimoto’s disease, further studies may be needed to determine which CTLA-4 incongruity is the causative agent.
#5: Vitamin D Receptor Gene
Vitamin D plays a key role in your immune system.
Acting as a natural immune system modulator, vitamin D binds to the vitamin D receptor gene, activating and regulating multiple cellular pathways that enhance cells like CTLA4.
Via the vitamin D receptor gene, vitamin D regulates calcium metabolism, cellular growth, proliferation and apoptosis, and other immunological functions.
Studies have reported that genetic variations of the vitamin D receptor gene may be related to different autoimmune disorders, including Hashimoto’s disease.
#6: Cytokine Genes
Cytokine genes are a category of small protein substances that are secreted by certain cells of the immune system and have a specific effect on the interactions and communications between cells.
Due to their small size, cytokines activate cytokine receptors in the cytokine gene on the target cell surface.
Some cytokine genes have been found to influence the presence and severity of Hashimoto’s disease by increasing a cell’s quality to be toxic to other cells, promoting the destruction of the thyroid in Hashimoto’s patients.
Additionally, certain genetic variations of the cytokine genes that inhibit cytokine production were
observed more frequently in people with severe hypothyroidism than in those with mild cases.
5 Non-Genetic Risk Factors for Developing Hashimoto’s Disease
#1: Sex
Studies have reported that women are more likely than men to develop Hashimoto’s disease.
While key indicators have yet to be identified, many researchers believe the prevalence of two X chromosomes containing several immune-related genes increases the chances of the presence of positive TAbs in women, making women four to 10 times more likely to develop Hashimoto’s than men.
Others believe that due to the presence of two X chromosomes in women, women have a higher immune response than men, increasing the risk of developing autoimmune diseases.
Pregnant and postpartum women are also more likely to develop Hashimoto’s as the normal shifts in immunity and hormone function can cause the thyroid to become inflamed or trigger the immune system to attack the thyroid gland.
#2: Age
Research shows women between the ages of 30 and 50 are more likely to develop Hashimoto’s disease.
Diagnosing Hashimoto’s disease early on is often challenging and may take time until symptoms become more noticeable since the severity of the disease tends to worsen over time as thyroid activity deteriorates.
However, patients can still exhibit signs and
symptoms early in the course of the disease while displaying normal results during hyperthyroidism testing due to the intermittent nature of thyroid gland cell deterioration and
mitosis.
#3: Medical Treatments
Certain drugs used to treat conditions unrelated to the thyroid have been shown to display side effects that impact thyroid function.
The following medical treatments have been reported to influence susceptibility to developing Hashimoto’s disease:
These drugs can exacerbate thyroid autoimmunity by increasing TAb positivity in susceptible individuals by:
- Triggering immune response
- Suppressing T-cell function
- Activating immune cells; and
- Stimulating cytokine release on thyroid cells
#4: Chemical Exposure
Exposure to carcinogenic chemical compounds commonly used in a variety of industrial and consumer products, like polyaromatic hydrocarbons or polyhalogenated biphenyls, has been reported to trigger thyroid autoimmunity in studies on animals and humans.
A study of residents living in a polluted district in East Slovakia found exposure to polychlorinated biphenyls was associated with TAb and hypothyroidism.
Another study found a significantly higher occurrence of Hashimoto’s-causing TAb positivity in residents living near a steel industrial area in São Paulo.
Findings suggest that people living in low-income areas are more susceptible to developing Hashimoto’s disease due to the proximity of the neighborhoods to industrial areas.
Though strong evidence exists that links exposure to toxic chemicals and thyroid autoimmunity, the exact method by which this occurs hasn’t been established.
#5: Ethnicity and Race
Though anyone can develop Hashimoto's disease, it's most commonly reported among middle-aged women of Caucasian descent.
Though people of European or Caucasian descent are more likely to develop Hashimoto’s disease than those of African and Hispanic descent, many studies have found that Hashimoto’s disease also affects more people of Asian descent.
The largest National Health and Nutrition Examination Survey (NHANES III)
study reported that Hashimoto’s disease was significantly higher in
Japanese and Caucasian Americans than any other race.
HealthierU: Providing a Holistic Approach for the Treatment of Hashimoto’s Disease
If you know or suspect you may have Hashimoto’s disease, making changes to your diet can help keep the uncomfortable flare-ups in check.
At HealthierU, our holistic approach to treating Hashimoto’s disease utilizes the power of nutrition by fueling your body with the right foods to manage symptoms.
Let Dr. Sergi guide you through a custom, comprehensive nutrition plan to restore harmony within your immune system, body, and mind.
Schedule your consultation today and learn how HealthierU can supplement your Hashimoto’s treatment with the right nutrition plan to get you back on track to living a symptom-free life.